In this post I would like to share some thoughts about rule 3.
This is the rule that many people scratch their head over, mainly because it can be difficult to see, but also because it doesn’t come up that often (and generally only in more complex cases). Therefore, if you’re used to testing routine cases you may not have to think about rule 3 very much. That’s why it’s good to refresh your knowledge so that you don’t miss it when it does come along. Completing rule 3 means that your hearing test will be more accurate; the end result may affect your diagnosis and also your hearing aid prescription.
How does Rule 1 differ to Rule 3 in masking?
We know that Rule 3 is only needed when Rule 1 has not been carried out and that both involve air conduction masking. But why?
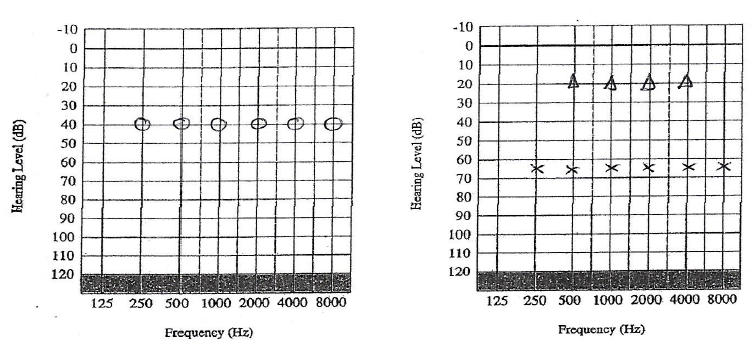
Masking is carried out when there is a difference of 40dB between cochleae when using headphones. When we look at Rule 1 the difference between the two cochleae are obvious:
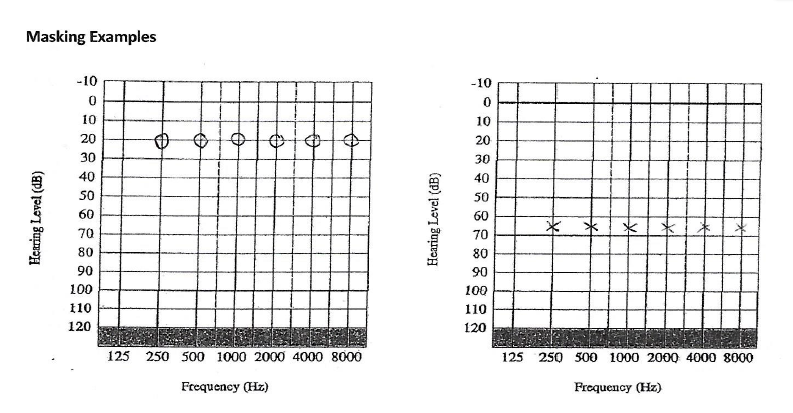
We mask the air conduction, and find the following:
Rule 1 was carried out at all the frequencies as there was a difference of >40 dB at all the frequencies between the 2 ears. Headphones were used and the left ear was the test ear, and the right ear was the non-test ear, to be masked.
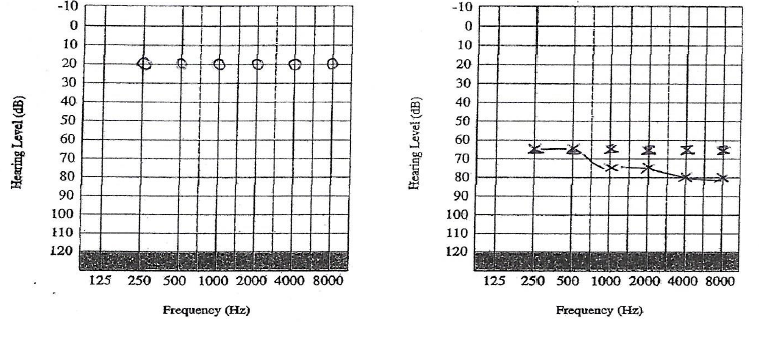
However, the difference between the two cochleae can be hidden when the non-test ear has a conductive component. Say for example the same patient as above comes back a few weeks later with a hideous cold that has affected his right ear.
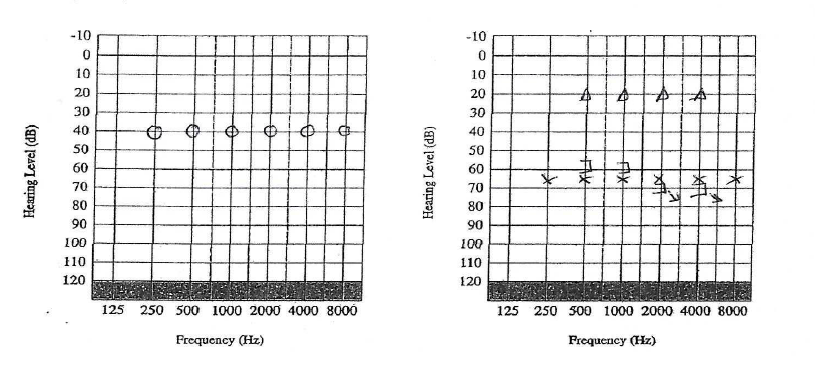
There was no need to do air conduction masking in this scenario (Rule 1 not required).
Bone conduction was carried out on the worse ear:
As the there was an air bone gap of >10dB between the air and bone conduction thresholds (Rule 2), bone conduction masking needed to be carried out at 0.5, 1, 2 and 4 kHZ. The left ear was the test ear using bone conduction, and the right ear was the non-test ear, to be masked.
Once bone conduction was completed, we could see an asymmetry once again:
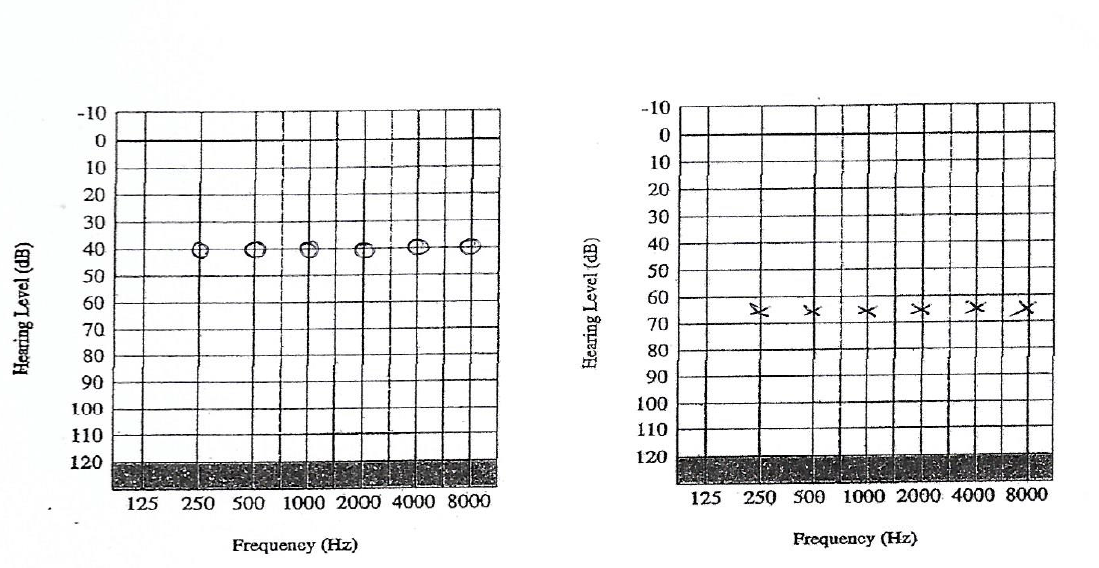
In this case we could only see that the right cochlea was >40dB better than the left cochlea because bone conduction had been completed. So we went back to using headphones again and masked the air conduction, with the masking noise in the right ear (non-test ear), and retested the hearing thresholds on the left ear (test ear). This revealed the following:
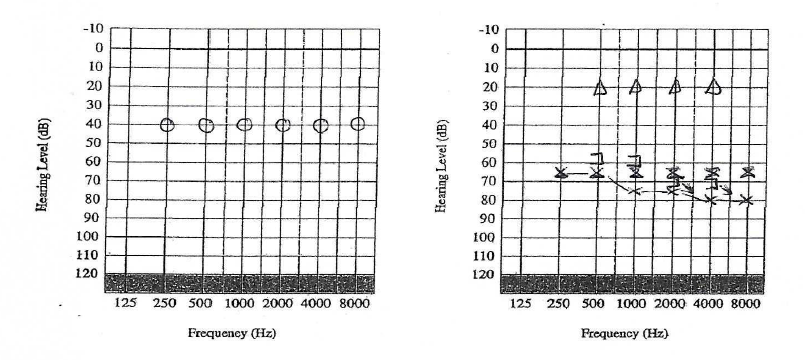
Moderate to severe sensorineural hearing loss on the left. Mild conductive hearing loss on the right.
Rule 3 explained? (Some tips):
-
Rule 3 is usually required because the non-test ear has a conductive component
-
The asymmetry that is present between the 2 cochleae (as you would visibly see in Rule 1) is hidden until you carry out the bone conduction. That is why you only carry out Rule 3 if Rule 1 has not been carried out.
-
Rule 3 is often missed because the BC that relates to the better ear (non-test ear) is recorded on the side on which the BC is placed (worse ear). Therefore you have to think to which ear the not-masked BC belongs to.
-
Although you check the BC to ascertain an asymmetry, you don’t use the BC in your masking procedure – you are masking the AC thresholds only.
-
At frequencies where no b-c thresholds have been measured – if there is a possibility that a-c threshold at these frequencies (including 250 Hz and 8000 Hz) are not the true thresholds, they should be masked.
If you have any questions please send an email to admin@tjaudiology.com and either Tracy James or Louise Hart will get back to you