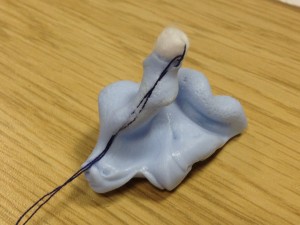
Louise Hart joins Tracy James to deliver tinnitus and hyperacusis services to adults and children from October 2020. She will also be providing her expertise in our training courses delivered to provide British Society of Audiology Certificates in impression-taking, hearing surveillance and audiometry and tympanometry.
Louise says ‘ I am excited to be providing more independent work, alongside my NHS work. I really enjoy training and have pride in helping individuals enable their skills to the recognised standard of the British Society of Audiology. We will be training GPs, teachers of the deaf, assistant audiologists and any professional who works in the hearing industry, and I look forward to meeting our new delegates at the next course in Newbury.’
‘With regards to tinnitus, I will be providing the only independent tinnitus and hyperacusis management service in West Berkshire at Tracy James Hearing. We know the earlier we intervene in helping people manage their tinnitus and hyperacusis the more successful the outcome for them’
Despite research on drug or physical interventions on tinnitus, at present none seem to consistently reduce tinnitus well enough; this is why management techniques are used to combat tinnitus. For over 20 years chronic pain sufferers have successfully been using cognitive behavioural techniques to manage pain, and we now have more studies showing the same success with tinnitus.
Louise will tailor a programme to you to help your tinnitus and/or hyperacusis; these can be provided face to face or through video consultation. For further information on tinnitus and or to book an appointment, go to Tracy’s website tjhearing.co.uk.
For further information on audiology training courses, go to tjaudiology.com