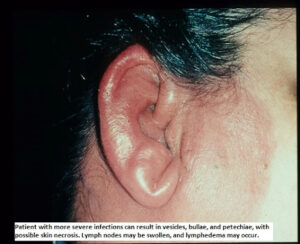
We often see skin pathologies on the Auricle but rely on dermatology or the client’s GP to know whether it is of concern or not. It is not in our remit to diagnose. However it is important that we are able to recognise these skin conditions and alert the client to the need for them to be investigated, if they haven’t already. Remember peoples ears vary and so can the presentation, depending on the shape of the ear and any previous history or ear surgeries. I have attached pictures and videos below that help us in the field of audiology to better able to distinguish different issues with the pinna and auricle.
Otitis Externa/Dermatitis Psoriasis/ Eczema – Pinna and Concha
There are few different types of eczema that individuals can be prone to. Some are related to age, some oiliness of the skin and others due to contact. https://eczema.org/information-and-advice/types-of-eczema/ear-eczema/
Atopic Dermatitis
The skin here on the ear or beside the ear (behind the ear or on the face is dry, itchy and red or darker than a person’s usual skin colour, depending on skin tone. Eczema in this area can cause fissure or cracks in the skin, which can then easily become infected. Sometimes eczema can affect the whole of the pinna and concha bowl and track down the ear into the canal. (as shown below)
https://dermnetnz.org/images/otitis-externa-images has supplied almost all of the below images

Seborrhoeic dermatitis
Occurs because of an over-reaction of the skin’s immune system to an overgrowth to a yeast called malassezia that lives on the skin. The ear is particularly prone to this like the scalp because of higher levels of oil on the skin in these areas. People who have this type of eczema often have dandruff on their scalp and itchy, flaky skin with a yellowish, greasy scale in on their face and near eyebrows etc. Around the ears, you will see it cause an inflammation of the ear canal (as shown below) and often also found on the hairline behind the ear.

Image From: https://skinsight.com/skin-conditions/seborrheic-dermatitis/teen/
Asteatotic Eczema
As we get into our more senior years our ears are more vulnerable to changes in weather and temperature, which can lead to dry, scaly and itchy skin . Over-washing, cold or windy weather, central heating, low humidity indoors and air-conditioning and not drinking enough water doesn’t help either.
Contact Dermatitis
Its what its says above, the skin has been irritated but something it has come into contact with, the skin becoming dry, itchy and red or darker. Contact dermatitis around and i inside the ears may occur from an irritation to a shampoo, hair gel, hair spray, perm solution, hair colourant, earrings , face creams etc.
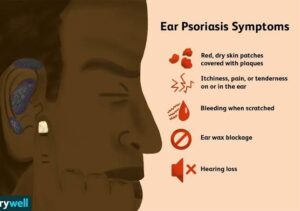
Psoriasis
Image: Verywell / Nusha Ashjaee
Psoriasis is a chronic disease that is caused by an overactive immune system and is associated with inflammation throughout the body. Symptoms may resolve and recur throughout a person’s life.https://www.psoriasis.org/about-psoriasis/. Around 39% of people living with psoriasis on the face have it in or around their ears (and hairline). Psoriasis plaques appear as raised, inflamed, and scaly patches of skin that may also be itchy and painful. On paler skin, plaques typically appear as raised, red patches covered with a silvery white buildup of dead skin cells or scale. On darker skin the plaques may appear darker, thicker, and more of a purple or grayish color or darker brown. People with psoriasis often produce more dead skin in and around the ear canal, causing increased skin and wax debris and therefore may need more frequent wax removal.
Image from: https://denizyilmaz.com.tr/en/external-ear-canal-disorders/

Cancerous Lesions on and around the Pinna and Outer Ear
One of the places we never put sunscreen is on our ears and this is one of the first places that skin cancers can develop. if you client has an unexplained sore on the ear or abnormal pigmentation that has not been checked then please ensure that they follow this up with the GP and ideally report in a letter to the GP. A study from one tertiary centre found in their centre that squamous cell cancer, including early-stage ones, comprised 72% of the ear cancer cases treated at the facility from 2009 to 2014. Patients with basal cell cancer made up 23%. Rare tumor types included melanoma (4.04%) and atypical fibroxanthoma (0.1%). https://pmc.ncbi.nlm.nih.gov/articles/PMC7580161/pdf/10.1177_2473974X20964735.pdf
:max_bytes(150000):strip_icc():format(webp)/VWH_Illustration_Signs-of-Cancer-on-the-Ear_Illustrator_Jiaqi-Zhou_Final-321afe46901e4324b6dc35bdaa1129fb.jpg)
Cancers on the pinna and concha almost always start out as skin cancer. The most common types you will see on your client’s ears are basal cell carcinoma and squamous cell carcinoma. Basal cell and squamous cell skin cancers if caught early can will require removal but not be life threatening. It is also possible to develop melanoma skin cancer on your ear, but this is much rare (and of more concern).
Basal Cell Carcinoma

Image From: https://www.pcds.org.uk/clinical-guidance/basal-cell-carcinoma-an-overview
Basal cell carcinoma is the 2nd most common form of skin cancer to show up on the ear. They are usually slow-growing and rarely spread past where they first appeared unless left for a long time, and then more margins will need to be removed. The estimated lifetime risk for BCC in the white population is 33-39% for men and 23-28% for women. With darker skins around half of all pigmented lesions that appear brown or black. Over time, the growths may bleed or ooze. A sore on the ear that never seems to heal properly could also be a sign of basal cell carcinoma https://www.pcds.org.uk/clinical-guidance/basal-cell-carcinoma-an-overview
Squamous Cell Carcinoma


Squamous cell carcinomas can be found on the pinna, concha as shown in the above images from Healthline and DermNet or even in the ear canal (the attached link below has images of canal squamous cell carcinomas’) https://onlinelibrary.wiley.com/doi/full/10.1002/lio2.330 https://pmc.ncbi.nlm.nih.gov/articles/PMC6081282/
SCC are generally faster growing than basal cell cancers. They begin in epidermis cells which produce keratin
Most SCCs develop on areas of skin exposed to the sun. (we don’t put sunscreen on our ears) They can also develop on scars, areas of skin that have been burnt in the past, or that have been ulcerated for a long time. Fair skin increases the risk.
SCCs don’t often grow wider but may grow deeper, leading to symptoms like ear pain, discharge, or even hearing loss and dizziness if it spreads to the temporal bone.
What to look for:
A persistent sore or spot on the ear flap that does not heal
Pink, scaly, or crusty lumps
Bleeding from the spot
Ear discharge, which may initially be mistaken for a otitis externa. Discomfort or pain in the affected ear
Melanoma
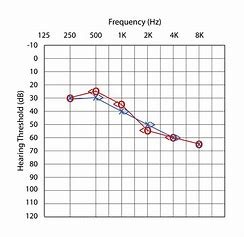
Auricle melanomas’ are rare, corresponding to 1%–4% of , 76,380 cases in 2016 in one article in the USA. It affects mostly men in their 50’s (less common in women) and those with fair skin and often is found on the helix.

Images above and below From: Ear melanoma: a four-case series Author:Lara Martins Fiorio,Lucia Martins Diniz,Karla Spelta,Bruna Anjos Badar https://doi.org/10.1016/j.abd.2020.08.003
Melanomas can appear as an irregular changing spot, mole. An irregular changing spot or mole or a sore that doesn’t heal. Symptoms can include a new mark with abnormal color or shape, a lump, or a sore that oozes, bleeds, or itches. Can appear as a tan, brown, or black growth, or as an non-pigmented variant

If melanomas are caught early the 5 year survival rate is 99%. If not caught before they extend onto the lymph nodes then the survival rate reduces from 66% if lymph nodes only; to 26% if beyond the lymph system.https://www.medicalnewstoday.com/articles/ear-melanoma#causes