UPDATED 28.8.25
Since I wrote this blog, I have been researching further into the topic. Along with training, I still work clinically and over the last few years we have seen a significant increase in cases of Otitis Externa (OE). This is something I am now seeing weekly instead of infrequently. In the last week we have seen at least 6 clients with OE out of the 25 clients we saw. Many of whom were new clients to us. This has been seen by others in clinical practice and researchers alike. This prompted me to do even more research on the topic to see what else I can do with my clients, and to share with you what I do in my clinical practice already.
ENT Surgeons at Freeman Hospital in Newcastle UK have also noted the same issue. 40,000 cases of otitis externa are diagnosed by UK GP’s each year. They have seen a 61% increase of inpatient admissions for severe episodes of OE between 2002 to 2017. Freeman Hospital : ENT Department Research on Otitis Externa
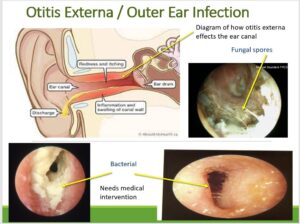
What is otitis externa? Firstly, it’s in the name Otitis is Latin for ear and Externa is external ear and it is an inflammation/infection of that area (generally it just the ear canal). Some people call it swimmers’ ear. But be aware this can mean something different depending on the region you live in the UK or what country you are in.
What causes Otitis Externa?
We aren’t exactly sure but some of the possible causes are:
- Damage to the skin in the ear canal (caused by cotton buds, scratching or poking) can cause inflammation and infection.
- Water can get into the ear canal during swimming. The stagnant water triggers an infection (Remember all water contains pseudomonas bacteria) . This often happens if there is a lot of wax and the water gets stuck behind the wax.
- Hot, humid weather makes inflammation of the ear canal more likely to develop.
- Skin conditions such as eczema, or psoriasis, can make someone more likely to get problems with the ear canal.
- Diabetes, radiotherapy (near the ear) and immune and conditions that effect the immune system can also make the client more prone to infection.
Who is at higher risk what does the data show?
- Research shows that clients with eczema and dermatitis are at higher risk
- As are clients with systemic allergies
- Clients with diabetes
In fact research shows that OE is often due to an allergy reaction. This may be to water, hearing aids, irritation from wax in ear or soaps. These are all things to consider.
How to spot the signs?
- In general the first sign your client will complain of is persistent itchiness and dry flaky skin around he canal and their may be some redness too.
- Smell – this like off cheese or smelly socks (it stays with you when you smell it!)
- A watery discharge from the ear canal (this can change later when its whiter)
- Discomfort moving the jaw when chewing or speaking.
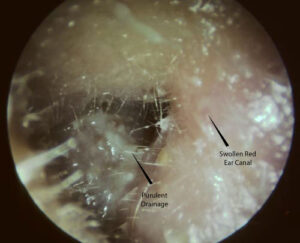
- The ear canal starting to close up due to swelling and inflammation.
- Reduced hearing due to the canal being full of discharge or the canal is completely swollen
- Fungal spores are also a form of otitis externa. These will be either white and furry or black (see picture below)
What should you do as an ear care professional?
Firstly, if they are seeing you for ear impressions or a hearing test, then you need to send them away. The swollen canal will prevent an accurate impression and you can’t do a hearing test as the risk of cross infection is too high.
What if they are seeing you for wax removal?
It may be that you can’t see it or smell it till you have removed some wax. If this is the case then remove as much as you can comfortably for the client. This will give any intervention a better chance of working, as you have made the canal clear of as much debris and discharge for antibiotics to work on the skin. Remember the ear may be sore so you may have to work slowly and gently and you not be able to remove all of it. (Please note irrigation is not an option here only microsuction; as water from irrigation will make things worse).
Remind them of good aural hygiene. No water near the ears and no touching of the ears whatsoever.
If the otitis externa has been caught early, you can suggest the use of Earcalm/ Otinova from the pharmacist, to stop the infection early on. But please ensure that they leave it a day or two after the wax removal so that the ear has time to recover from the removal and be less sensitive.
But only if there is NO PERFORATIONS. If perforations are present then they will need to be seen by a GP or ENT of oral medication options. Ear drops are CONTRAINIDICATED, as they may enter and damage the middle ear.
Once you have removed the wax and discharge, refer the client to the GP if you feel the over the counter medications wont work. They may prescribe eardrops or spray. Often, it’s a combination of an antibiotic to treat any infection, and a steroid to reduce the inflammation and itching. The treatment usually lasts for 7 to 10 days. They need to follow the prescribed course. If they return to you because the treatment hasn’t worked, then you need to recommend that the nurse or GP take a swab sample, as the antibiotics may be the wrong type for the bacteria present.
Key messages from Freeman Hospital Research in 2022
• Most patients with otitis externa (OE) have been treated with oral antibiotics (this shouldnt always be the first line defence)
• Ototopical drops are underutilized. Whether this be Earcalm, Otinova or prescription Otomize.
• Many patients are not told, or fail to retain, advice on water precautions. (This is critical in reducing infections).
- Antiobiotics are being over prescribed, increasing risk that the OE, whether fungal or bacterial of becoming antibiotic resistant.
• Many patients have associated risk factors including dermatitis and allergies.
• Most patients referred with OE have anatomically normal ears.
• Most patients are suitable for management in community aural care clinics.
The take home from the research is that early diagnosis of otitis externa, the use of non-prescription drops/sprays and clearing out any discharge before use of the drops, reduces the need for medical or ENT intervention with antibiotics and/or other interventions.
Medications and Prescribing Guidelines for Otitis Externa
To understand the prescribing pathway otitis-externa-acute-and-chronic.pdf from Nottinghamshire Area Prescribing Committee is a very helpful document as is Ear | Treatment summaries | BNF | NICE
Client Information Sheet on Otitis Externa
Outer ear infection or otitis externa ENT UK is a useful sheet to give to clients.
Information Sheet for Audiologists
https://www.entuk.org/_userfiles/pages/files/guidelines/global%20ent%20guidelines/otitis_externa.pdf . Is a useful sheet for the audiology professional seeing a client with otitis externa.
How I have changed what I do in clinic
After researching further in the last few months. I do the following.
- I strongly suggest the use of Earcalm a few days after irrigation or microsuction particularly if the ear looks more red than I would expect. Please give the ear time to recover and get its natural oil layer back on the ear canal skin before using the Earcalm.
- I generally wont remove wax if fungal spores are obviously present as this may spread the spores. Unless the ear canal is completely blocked with fungus (then drops are less likely to work effectively) then I would remove the debris. Pharmacies can prescribe over the counter Clotrimazole (Canestan drops) which is an antifungal to get rid of it. You only need a few spores to move or remain and the infection will start again within days.
- I clean out as much discharge as I can if OE is obviously present.
- I strongy recommend anyone with allergies or skin issues around the ear to by medical swabs and clean their aids before they insert them
- Suggest rest times from hearing aids to let the ear breath if client has very occluding moulds.
- Do not get the ear wet until the infection is well and truly gone.
- If I suspect that water is causing an allergy reaction, I will strongly suggest swim plugs be worn during showering and swimming; that the plugs are cleaned after use. Or they can use cotton wool with vaseline on the cotton wool as a ear plug (fresh one each time)
- The use of acidifying ear spray (EarCalm) and/or Earol Swim drying drops (70% isopropyl alcohol) after swimming or showering. According to Neil Fergie ENT in Nottingham, divers will often use a home made remedy of 1 part white vinegar to 2 parts isopropyl alcohol – acts as a drying and acidifying agent (natural ear canal pH is acidic)
- If they are someone that also produces lots of wax they will need to get wax removed more frequently so that water cant get trapped behind it.
HYGIENE, HYGIENE, HYGIENE
Lastly
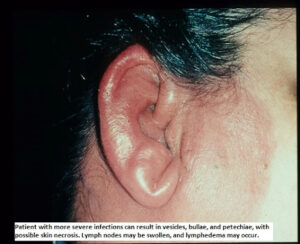
If the canal is swollen shut and the pinna and the concha are also swollen then the otitis externa has developed into cellulitis, this is a rare occurrence/side effect . (This may have occurred due to the client scratching the already infected ear and adding another bacteria). They will require intravenous antibiotics for this, so in this case suggest they attend A+E or Emergency ENT clinics as this cannot be given at a GP surgery.